Service development and innovation (MRI physics)
The group is also instrumental in enabling and developing advanced MRI techniques for clinical use - we encourage innovation and improvement to benefit our patients and work closely with our radiology colleagues to deliver a high-quality clinical MRI service. We are part of the MRI protocol group, and as part of this group we are pushing forward the boundaries of clinical MRI. Here are a few of the service development projects we are involved in:
Cryoablation
For patients with remaining lesions, cryoablation can be a suitable treatment, by freezing the lesions to destroy them. MRI is used to guide the placement of biopsy needles and cryoablation needles for treatment of the prostate. Our work included validating the depiction of the ice within the images to provide clinicians with confidence that they are sparing sensitive tissues and covering the target region.
Radiotherapy planning
Patients for radiotherapy have a “planning scan” before treatment starts. This is to determine the location of treatment target, and also of sensitive adjacent tissues which should avoid being in the radiation field. These scans also enable a map of tissue “electron density” to be calculated, which is needed for calculating tissue radiation doses. The planning scan is normally a CT scan, owing to its good geometric accuracy, ability to create electron density maps, and widespread availability. However, MRI provides much better soft tissue contrast than CT. Along with a number of other hospitals we are developing the addition of MRI planning scans to improve target definition in several patient groups. This requires the use of MR-compatible positioning aids, to ensure that the position of the patient and their internal organs are the same for CT, MRI and treatment. MRI scans also need to be optimised to minimise distortions.

The image above shows some of the equipment used for radiotherapy planning scans, including the flat couch top, the coil bridge to keep the MRI detector coil from distorting patient anatomy, and the knee and ankle supports whose position and angulation can be specified for each patient exactly as for the treatment position.
fMRI for characterisation of CSF flow
Our team has been developing a new way to use resting-state functional MRI (fMRI) brain scans to help patients with a condition called hydrocephalus, where there's too much cerebrospinal fluid (CSF) in the brain. We use fMRI scans to check if there are any blockages in the pathways where CSF should be flowing. This is essential because if CSF is not drained promptly, it can induce higher pressure and cause damage to the brain tissue.
We've designed a special scanning technique that helps us determine whether the pathway of CSF drainage is patent. When fresh CSF enters the image acquisition area during the scan, it makes the MRI signal within that region light up, particularly for the edge slices, which is a phenomenon known as “inflow effect” or “time-of-flight effect”. This helps us determine if there are constant CSF flow within that region.
We apply fMRI to check how well a surgery called endoscopic third ventriculostomy (ETV) is working. This surgery creates a new pathway for CSF to drain. In addition, we also measure heart rate and breathing to see how these physiological measures are connected to the CSF flow in the brain.
DTI for neurosurgical planning
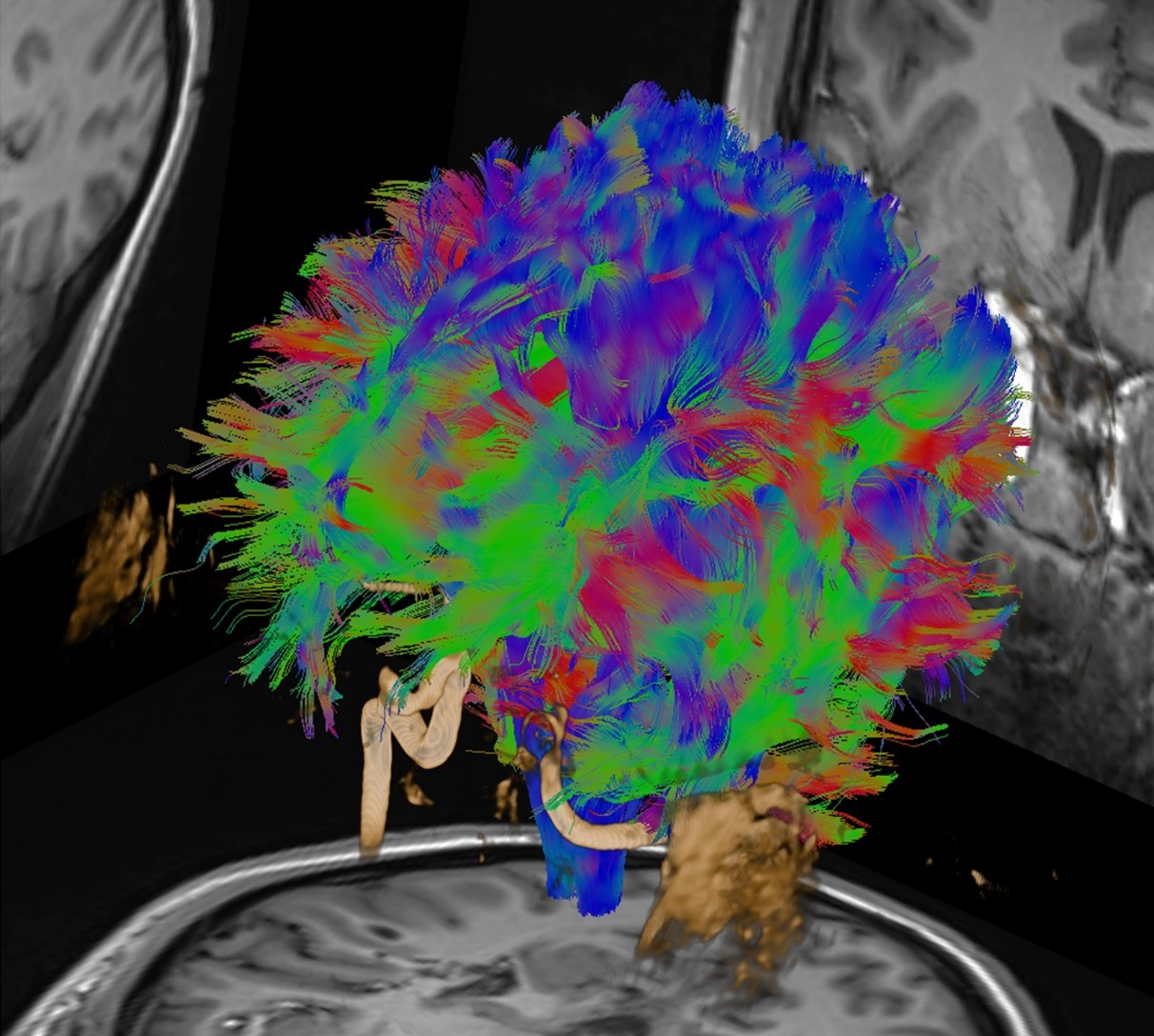
Our team is actively involved in establishing protocols for acquiring diffusion tensor imaging (DTI) data and checking data quality post-acquisition to ensure minimal motion artefacts or other acquisition issues. Our clinical DTI service assists surgical planning, which ultimately benefits patients with neuro-oncological, neurovascular, and neuro-functional diseases. We utilise a range of software tools for clinical applications from awake craniotomy, thalamotomy, deep brain stimulation, to the visualisation of Meyer’s loop.
There remains a crucial need to streamline communication about patient data quality. In collaboration with radiology, we are working to enhance the efficiency and accessibility of this assessment of image quality, integrating advanced imaging processing with the optimal utilisation of DTI data, and facilitating a seamless process for all the stakeholders. One of the recent initiatives at UHS is the MRI helpdesk, which is a ticketing system that utilises the existing IT service desk infrastructure and can be accessed by anyone with a UHS login. We hope to use this functionality to improve our imaging pipelines for these advanced MRI techniques, including DTI.
Magnetic resonance spectroscopy
Magnetic resonance spectroscopy (MRS) is a method to obtain biochemical information about tissues non-invasively. It uses the same equipment as MRI but instead of producing an anatomical picture it produces a spectrum, with different peaks reflecting the concentrations of different molecules.
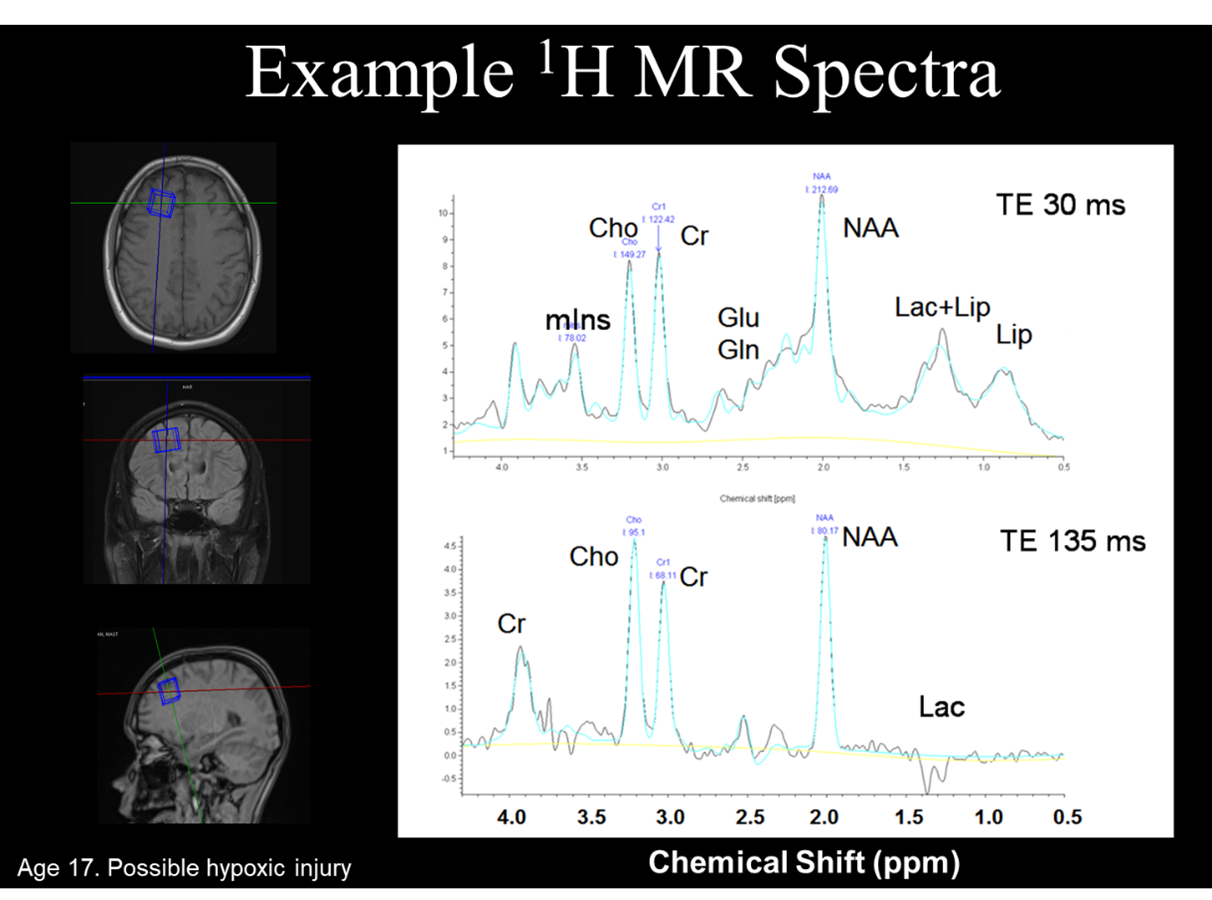
Magnetic resonance spectroscopy can sometimes detect changes in tissue biochemistry caused by disease, even when there is not sufficient change in tissue structure to be visible by MRI. For example, in babies who have suffered hypoxic ischaemic encephalopathy at birth the amount of lactate visible can help to predict the degree of recovery. A high glycine peak (not normally visible) is characteristic of patients with non-kenotic hyperglycinaemia. In other patients a mass lesion may be visible by MRI, but different metabolic fingerprints can help with the task of differential diagnosis.
QSM for visualisation and quantification
Quantitative susceptibility mapping is a technique that uses measurements of perturbations within the magnetic field to determine the underlying susceptibility distribution. This has potential clinical applications to monitor iron deposits within haemorrhage patients. It can also provide an additional MRI contrast type e.g. for visualising the nuclei within the thalamus.